Key Points
- Surgery is the treatment of choice for inguinal disruption (ID) when conservative treatment fails.
- Laparoscopic techniques provide advantages over open surgery, including faster rehabilitation and an earlier return to daily and full sports activities.
- Transabdominal preperitoneal (TAPP) repair should be performed bilaterally for better outcomes in ID cases.
Background
Inguinal disruption (ID) is a clinical condition characterized by chronic groin pain, predominantly affecting athletes, both professional and amateur. In medical literature, this condition has been referred to by various non-specific terms, including sports hernia, chronic groin pain, sportsman’s hernia, sportsman’s groin, athletic pubalgia, Gilmore’s groin, ice hockey groin, and pubic inguinal pain syndrome (PIPS). The Manchester Consensus Conference of the British Hernia Society (BHS) and the Doha Meeting worked to standardize the terminology, ultimately agreeing on the term “inguinal disruption” to define the condition.
ID is commonly seen in athletes participating in sports that involve frequent kicking and twisting movements while running. It accounts for approximately 6% of all athletic injuries. The condition affects between 0.5% and 6.2% of all athletes, with a higher prevalence in soccer players (males: 10–18%; females: 2–14%) and hockey players (13–20%). The median age of affected athletes ranges from 26 to 28 years.
Pathophysiology
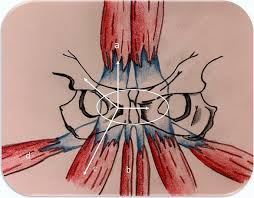
Unlike a true inguinal hernia, ID does not involve an abnormal exit of tissue through the abdominal wall. Instead, it results from a multifactorial pathogenesis, ultimately leading to weakness in the posterior abdominal wall within the inguinal region. This weakness creates abnormal tension in the inguinal canal due to unbalanced forces in the pelvis and surrounding musculature. The condition is primarily caused by repetitive and excessive forces applied to the inguinal and pelvic regions, particularly during lower limb movements involving the adductors, the lower abdominal muscles, and the hip joint.
Clinical Presentation
Patients with ID typically report unilateral groin pain at the pubic symphysis, which radiates to the scrotum, perineum, rectus abdominis, and adductor tendon, following specific nerve distributions. The pain is often accompanied by resistance or discomfort during ipsilateral hip adduction. Symptoms are exacerbated by athletic activities such as kicking, cutting, or sprinting, particularly during acceleration and deceleration, but they tend to improve with rest.
Physical examination typically reveals tenderness upon palpation of the inguinal region, just above the inguinal ligament and near the pubis. The pain is often worsened by coughing or performing the Valsalva maneuver. The presence of a visible or palpable inguinal mass suggests a true inguinal hernia rather than ID.
Treatment Options
Conservative Management
Initial treatment for ID generally involves conservative management, including:
- Rest and activity modification
- Physical therapy focusing on core strengthening and stabilization
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Corticosteroid injections in severe cases
However, when conservative treatment fails, surgical intervention is recommended.
Surgical Treatment
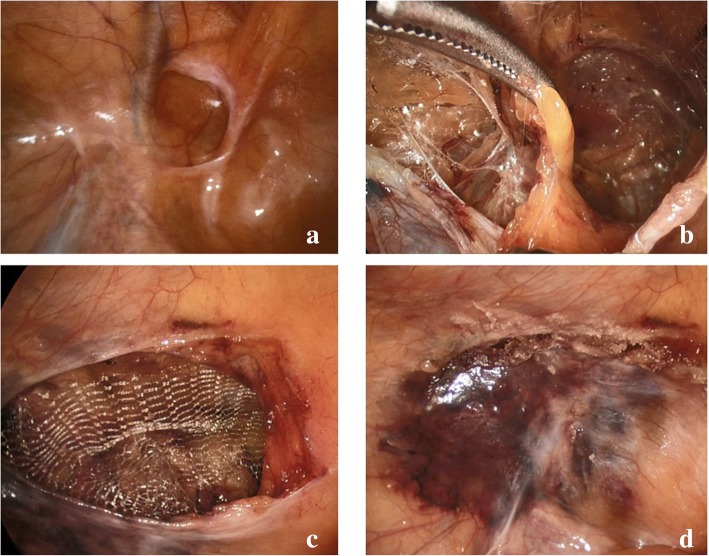
Surgery is the preferred treatment for persistent ID, particularly in high-level athletes requiring rapid recovery. Laparoscopic surgical techniques, such as transabdominal preperitoneal (TAPP) repair, offer distinct advantages over traditional open surgery, including:
- Reduced postoperative pain
- Faster rehabilitation
- Earlier return to normal daily activities and sports participation
TAPP repair is particularly recommended for bilateral treatment of ID, as it has been associated with superior long-term outcomes. The procedure involves reinforcing the posterior abdominal wall with mesh, reducing tension in the inguinal region, and stabilizing the affected structures.
Conclusion
Inguinal disruption is a significant cause of chronic groin pain in athletes, commonly affecting soccer and hockey players. The condition results from excessive stress on the inguinal and pelvic regions, leading to weakness and instability. While conservative management may provide temporary relief, surgical intervention—particularly laparoscopic TAPP repair—is often necessary for long-term recovery. With appropriate treatment, athletes can achieve full rehabilitation and return to their sport with improved performance and reduced risk of recurrence.